For details, please see here
For details, please see here
For details, please see here
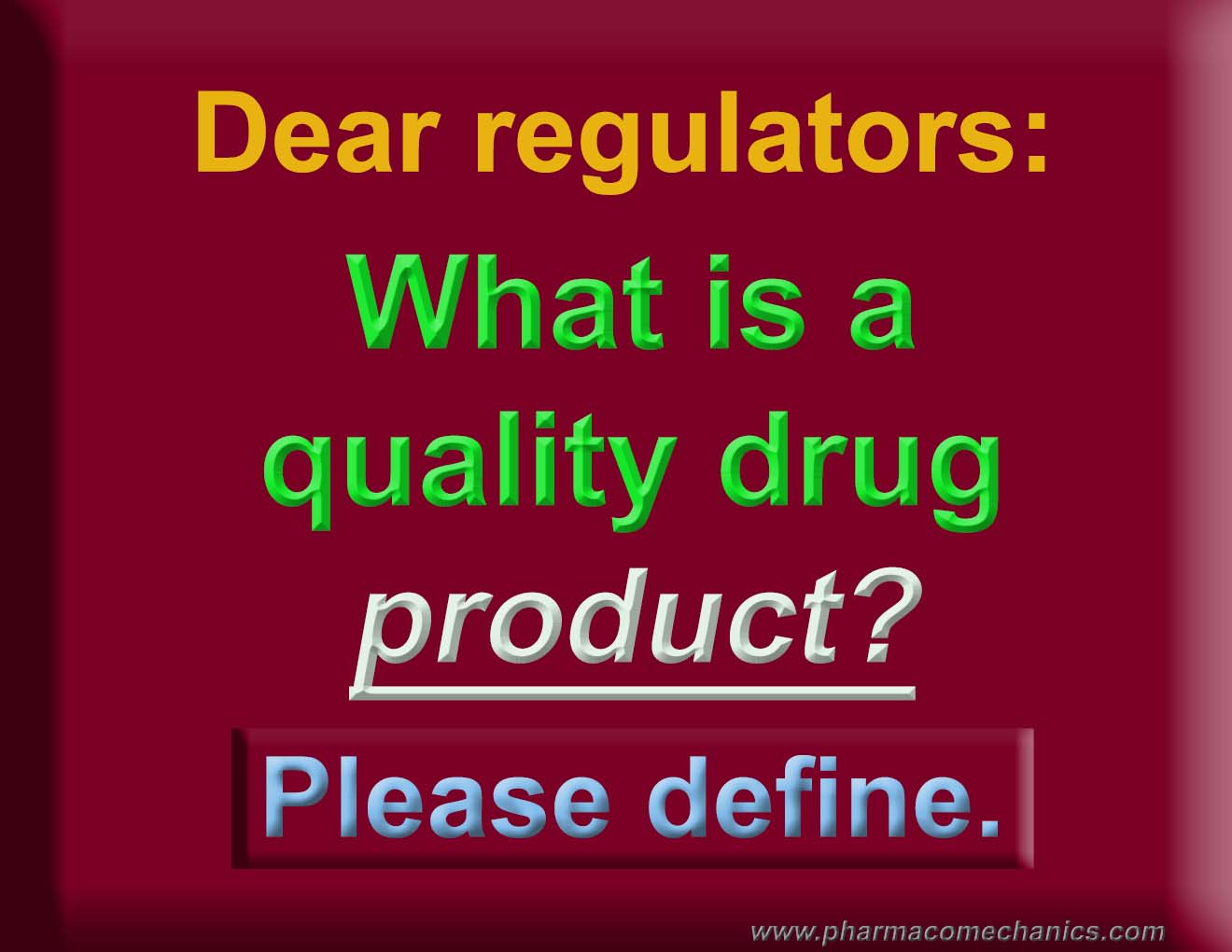
Use care in using dissolution testers, in particular the paddle and basket. These testers have never been validated and qualified for their intended use (link). Therefore, interpretation of the results obtained would most likely be misleading. This would be particularly true for assessing the quality of the products, which, at present, is an undefined parameter and objective (link).
Often people promote the use of current practices of dissolution testing as a regulatory compliant requirement, which to some extent is a correct but unfortunate practice. However, I believe such regulatory requirements will also be discontinued soon. Scientifically speaking, it is highly unlikely, if not impossible, that such practices can continue knowing that these testers are non-qualified and/or non-validated (a violation of GMP requirements).
Wish you all the best of luck and success in your professional and personal lives in the coming years.
For details, please see here
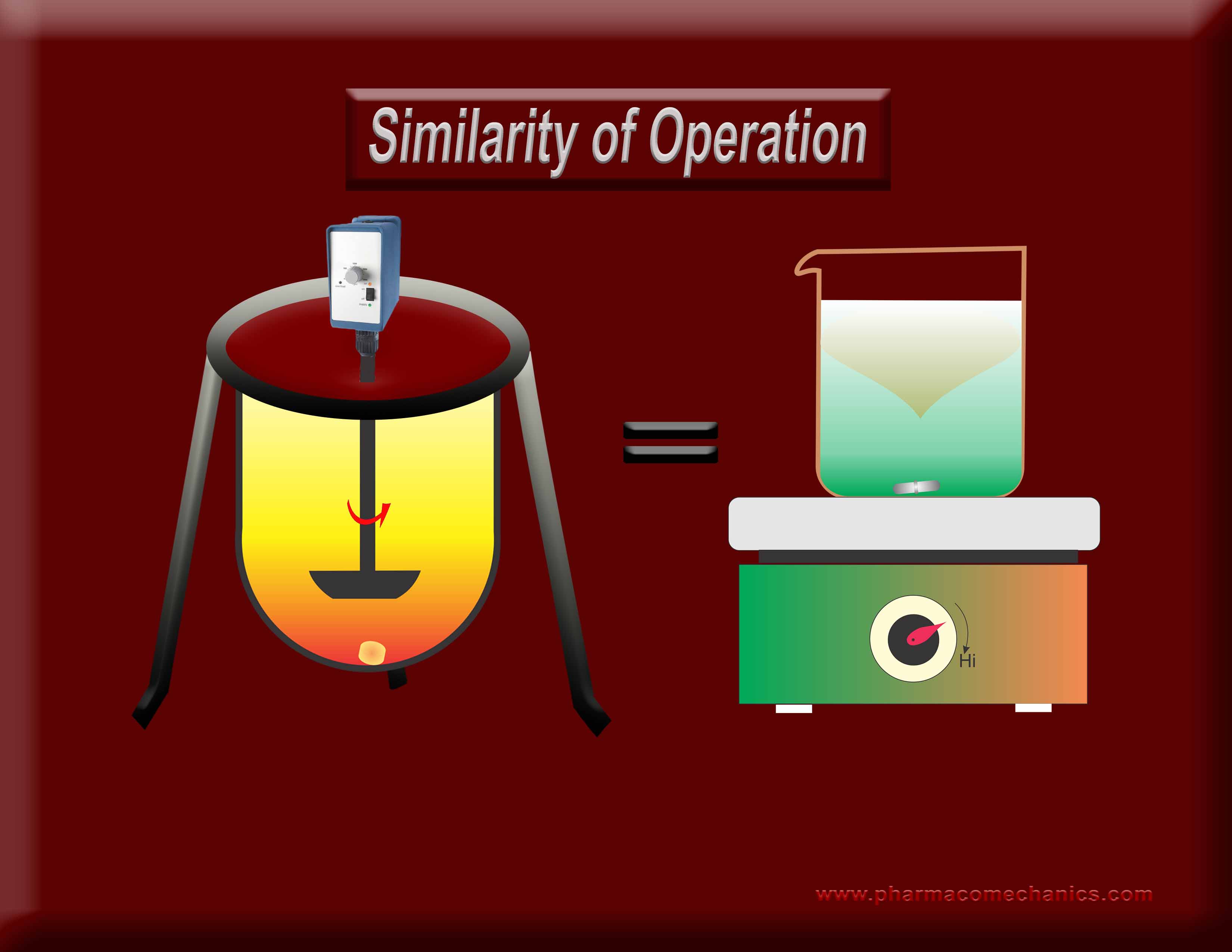
Why does one require an exhaustive standardization (calibration/PVT/Guidances/training etc.) for the operation of one stirrer type but not for the other when both are used extensively for the same purpose (dissolution)? Does it indicate a misunderstanding of the underlying concept? It appears so! To know more about why both of these stirrers are not suitable for DRUG dissolution testing? See here

This definition/metric needs to be included, as an assessment of practically all other factors such as safety, efficacy, manufacturing and its design and processes etc., are secondary to it. In addition, such a metric can easily be explained to the consumer/patient. For further discussions on the topic, please see the link.