… a product can have only one value for a parameter at any given time. It is not possible that the same product can have multiple values or characteristics of a parameter (drug release or dissolution) simultaneously.
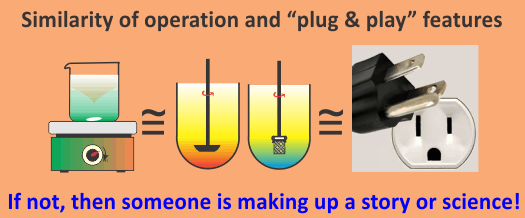
This is just like a tablet or capsule can only have a single weight at any given time, no matter which type of balance one would use to measure it. Or just like a dissolution bath can have one temperature at any given time no matter which type of thermometer one could use to measure it. Similarly, just like the content of a tablet/capsule (amount of drug) can have one value at any given time, no matter which type of analytical technique one would use to measure it. Of course, different techniques/methods may provide different precisions due to their nature, but results on average will be the same and technique independent.
The same tablet/capsule can’t have different weights at the same time. It is not possible that a dissolution bath can have different temperatures at the same time. It is not possible that a tablet/capsule can have different contents (amount of drug) at any given time.
If different balances, thermometers, or analytical techniques provide different results, this means that these measures the values of the intended parameters but something else. Such techniques or testers are considered unreliable and, as a common practice, are not used any further.
On the other hand, in drug dissolution testing practice, it is commonly accepted that each and every product can, and should, provide tester-dependent different dissolution values. A notable example in this regard is dissolution values for the USP prednisone PV Tablets, where paddle and basket provide two different drug dissolution values.
All four of the most commonly recommended dissolution testers are expected to provide different dissolution results for the same product. The analyst or formulator is free to choose, and rationalize, the one which suits his or her purpose. However, he or she will never be able to know the actual dissolution characteristics of a, or any, product. Presently, the drug release/dissolution characteristics are not product dependent but tester dependent. Obviously, one cannot establish the quality or bio-relevancy of any product as the results are not linked to the product but the tester.
It is such an unfortunate and bizarre practice and logic, not sure how this has been accepted and practiced for so long in the industry and regulatory environments. This is a serious anomaly that certainly requires urgent attention for correction.