The role of an (or any) analytical method validation (chromatographic/spectrophotometric) is to demonstrate that the method is capable of measuring an analyte accurately (accuracy, which includes specificity) and reliably (precision, which includes repeatability and reproducibility). In addition, if the analyte is expected to be in a wider range, e.g., zero to 100 %, which is usually the case in dissolution testing, then one has to establish that concentrations and responses have a linear relationship (linearity) by measuring responses at different concentrations.
All of the above-mentioned practices (tests) boil down to determining responses (UV absorptions or peak height/area for chromatography) against concentrations and are to be done in replicate (5/6 times) to be able to determine a standard deviation (variance) to establish confidence in the results. In short, if one has different solutions of 100, 50, and 25% concentrations (strength) of drug and measure their responses, which come out in the ratios as the concentrations (by doing it repeatedly 5/6 times), then the method has been validated.
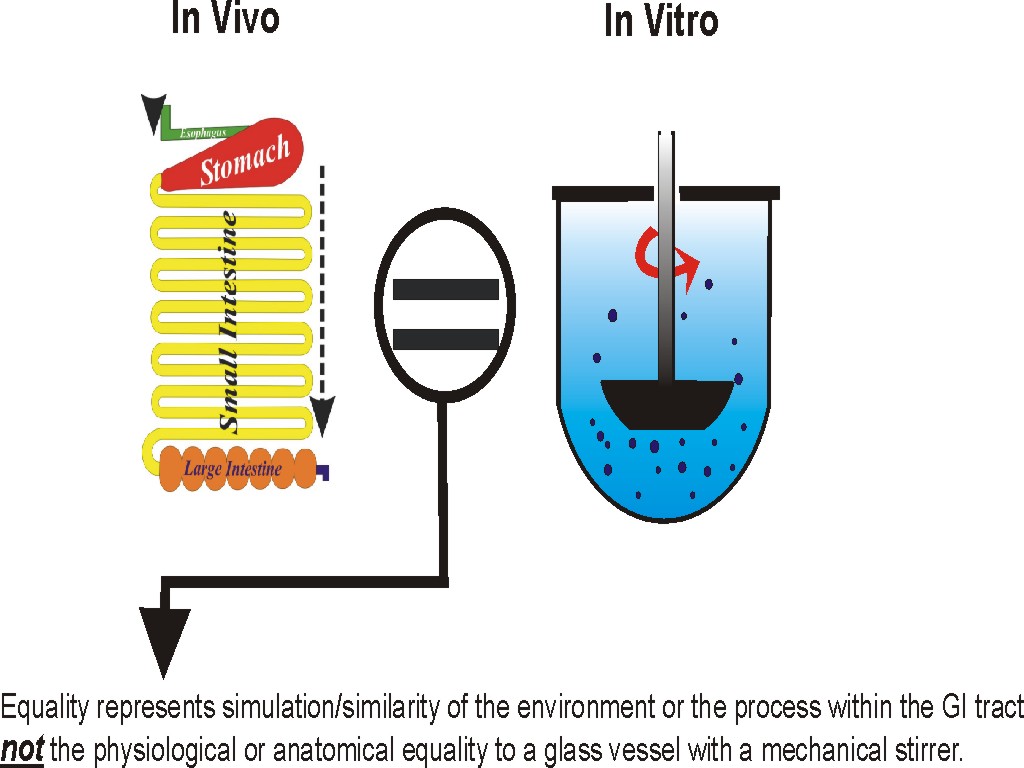
For drug dissolution testing, one has to demonstrate that if the drug is in solution, then the analytical method can measure it accurately and reliably. Therefore, to validate such methods, one needs to add the drug (“spiking”) in solution form to a dissolution testing apparatus, i.e., the vessel containing the required medium volume maintained at 37 ºC and spindle rotating. Samples are withdrawn and processed exactly as if these were from a product (filtration, dilution/concentration, extraction etc.), and responses are measured accordingly. If responses and concentrations are as one would expect (as explained above), then that dissolution method has been validated.
Then, one should be able to use this method (validated) to measure the dissolution of a drug from a product. Method validation steps are independent of drugs and products.
On the other hand, a method development exercise is drug and product-dependent. In (analytical) method development, an analyst needs to select appropriate parameters such as wavelength, chromatographic column, dilution, extraction steps, filters etc. Once such parameters are established, one then moves to the method validation exercise as a second step.