This chapter appears quite popular and is often cited for help and information concerning dissolution methods development and validation. However, if one evaluates it, even superficially, one should immediately realize that the chapter is based on invalid assumptions and false science. For example:
The chapter is meant to be helpful and useful in developing and validating a dissolution method. However, the problem is that a fundamental requirement is that one requires a reference product with known dissolution characteristics established independently for such a purpose. In this case, one requires a reference product, which should be approved for human use as the method is to be used for such a purpose, with known dissolution characteristics. The (dissolution) method development means that using valid scientific principles and testers, the developed and validated method would be able to provide an expected answer for the reference product. This developed and validated method will then be used for evaluating the test products. As, at present, a reference product with known dissolution characteristics is not available, therefore, it is not possible to develop and validate a dissolution method. It is simply a scientific impossibility.
Furthermore, the valid scientific principles and testers mean that developed and validated methods must be based on experimental conditions relevant to the applications of the method. In this case, the relevancy aspect comes from the physiological environment of the GI tract in particular intestinal. The only purpose of the test/method is to evaluate dissolution characteristics of a drug product in the GI tract. It is important to note that even for QC purposes, the method measures the dissolution characteristics for the GI tract. That is why most, if not all, pharmacopeial tests are conducted using physiologically relevant conditions as well. Therefore, the choice of experimental conditions must be physiologically relevant.
A fundamental requirement, in this regard, is that whatever experimental conditions one chooses to represent the GI tract environment, these should remain consistent from product to product or should be product independent, as does the GI tract environment. This is the second flaw (invalid science) of this chapter that it suggests and emphasizes selecting the test product-dependent experimental conditions. It will be impossible to determine a test product’s true and accurate dissolution characteristics using experimental conditions specific to the product itself. Furthermore, as the experimental conditions change from product to product, which is unlike the GI tract environment, therefore, such tests would be considered invalid for any purpose. No matter how one presents the argument, it will be an irrelevant evaluation method and test for product-dependent experimental conditions.
It is, therefore, critical to understand that the chapter cannot provide help or accurate information for developing or validating a scientifically valid dissolution method.
It is often suggested that to obtain appropriate dissolution characteristics of a product one may use or select an apparatus depending on the product attributes and/or desired release characteristics such as discriminating profiles, reproducibility, bio-relevancy, etc. Such reasoning dictates that the analyst/formulator should have an idea about the expected outcome of the results, whether based on an educated guess or from prior experimentation. Thus, by selecting a particular apparatus and/or its associated experimental conditions, one is trying to achieve the results reflecting one’s expectation.
For example, when one conducts an experiment using the paddle apparatus and finds dissolution results of a tablet product, and their variability, higher than expected while observing that some, or all, tablets are floating within the vessel during testing. Such behavior or experiment is commonly considered flawed or inappropriate. A common practice to rectify this “problem” is to either use the basket apparatus or a sinker to restrict this floating behavior assuming that this may be causing higher results and variability. This means that the analyst/formulator already has a preconceived idea/expectation about the results and variability of the product, and is trying to obtain those results by adjusting the means, in this case by using a different apparatus or a sinker. Obviously, the analyst is not determining dissolution characteristics of the product but achieving intended results by adjusting tester and/or associated experimental conditions. Read the rest of this entry �
Similar C-t (plasma drug concentration-time) profiles or BA/BE (bioavailability/bioequivalence) shows that the products (tablets/capsules) provide similar dissolution characteristics (all other things being equal). Therefore, for all practical purposes, the C-t profiles or BA/BE studies are the measures of in vivo dissolution characteristics of the products. Thus, by definition, assessment of in vivo dissolution becomes a product assessment/development tool while the same assessment tool becomes a quality control/assurance tool as well. It is scientifically and logically incorrect to separate or differentiate dissolution tests based on their use, i.e. as a product assessment/development tool and a “quality” control/assurance tool. The dissolution test remains exactly the same in both cases.
The same BA/BE test can be, and are, used during the product development stage as well as for comparing the performance of different batches of the same product. The BA/BE test does not change with the stages of product development and manufacturing.
Considering ethical reasons (testing in humans), cost and time, BA/BE tests can neither be conducted nor conducted routinely, but only for confirmatory purposes. However, for all other purposes, such assessments (during the product development stage and as a quality control tool during manufacturing of products) dissolution characteristics of a product are evaluated by in vitro dissolution tests. For all practical purposes, current drug dissolution tests are indeed used as a substitute of BA/BE, including for QC purposes such as pharmacopeial tests. Therefore, by definition, dissolution tests conducted as recommended are indeed bio-waivers. One does not require any further or special step to transfer a dissolution test to a bio-waiver status or vice versa. Stating otherwise would not change the reality or the fact.
If a dissolution test does not provide an in vivo relevant outcome, then the issue is with the dissolution test, and such a test should not be used any further until corrected. Requiring the use of dissolution tests that do not provide bio-relevant results for any purpose, cannot be justified on any basis, scientific or logical. It simply confuses reality, science, and people, and furthermore hinders efficient product development and manufacturing.
A drug dissolution test is one of the most critical and important tests used for developing and evaluating tablet/capsule products. However, unfortunately, as conducted at present, the test is also perhaps one of the most frustrating and the least value-adding tests one would use. The test is often promoted as a quality control test or tool as well, however, without defining or linking to a quality parameter/end-point. It is conducted using apparatuses that have never been validated for the intended purpose or objective, further increasing frustration. This article describes reasons for such practices and frustrations and suggests a simple approach to address the issues and concerns.
Please click here for the complete article
USP is seeking comments on a draft of the revised “General Chapter <1092> The Dissolution Procedure: Development and Validation” (link). Also provided is a Stimuli article: “Revision of <1092> The Dissolution Procedure: Development and Validation” (link), which is to be published along with the proposed General Chapter providing the background information for the suggested revisions.
The following provides some comments for the consideration of the USP:
(1) In general, the chapter appears poorly written, lacking focus and coherence of thoughts.
(2) The claims made in the article for method development or validationare nvaguely described and For example:
- The suggested apparatuses, particularly paddle/basket, are flawed (lack reproducibility and relevancy) and have never been validated. Therefore, developing or validating a method using such apparatuses would not be possible.
- Validating a method requires a reference such as a product, parameter value (e.g. dissolution results), and/or experimental conditions established independently. As such a reference is not available at present. Thus the dissolution methods cannot be developed in particular for setting regulatory/pharmacopeial standards such as for USP.
- The suggested method development approach appears to be a vague narration of selecting experimental conditions to obtain certain pre-defined or pre-conceived dissolution characteristics of a product, not for determining the true characteristics of a product. It is important to note that the choice of the experimental conditions should be linked to the GI tract environment and not the product. As the physiological conditions (or experimental conditions) remain constant or independent of the drug/product, one should not be able to vary experimental conditions. The suggestions in the chapter concerning selecting product-dependent experimental conditions are scientifically invalid for this purpose.
- In general, if given a blinded product sample, which is a normal and common analytical practice, no matter how thoroughly or attentively one would follow the suggestions provided in the chapter it would not be possible to determine relevant and/or true dissolution characteristics of any product.
USP should consider addressing the above-mentioned deficiencies before finalizing the chapter.
The most commonly reported results from dissolution testing for establishing the performance of oral products (e.g. tablets/capsules), in particular for immediate-release (IR) products, is that products should meet a criterion of not less than 80% drug dissolution within less than 60 minutes, mostly 30 minutes.
Let us assume that a dissolution test (n=6) provides the following results (% drug dissolved) at 30 minutes (96, 88, 65, 110, 66, 65; Ave = 82; RSD = 23%). Obviously, this test/product, with a Q of 80%, would not meet the USP tolerance at the first stage. However, with a bit of luck and the second round of testing of 6 units it may meet/pass the USP Tolerance criteria. For details, please see the link, in particular the data set in row one.
Let us discuss the interpretation of these observed results. Read the rest of this entry �
The quality of a solid oral dosage form, such as a tablet or capsule product, may be defined as its ability to provide expected and consistent (reproducible) drug levels in plasma/blood. The product is introduced into the GI tract through the oral cavity (mouth) to release its drug, which gets dissolved in the aqueous milieu and gets transferred into the bloodstream to produce its therapeutic effects.
This drug transfer from the GI tract to the bloodstream is described by different terminologies, often interchangeably, such as permeability, absorption and bioavailability of the drug. However, these terminologies have distinct meanings, and for clarity purposes, should not be interchangeably used. The purpose of this article is to describe and explain these terminologies to facilitate appropriate development and evaluation of the products in particular for the use of in vitro drug dissolution testing. Please click here for the complete article
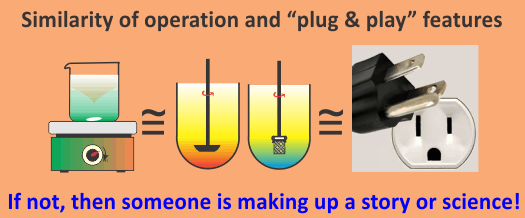
At the product development stage, the objective is to develop a product (tablet/capsule) having certain desired drug release/dissolution characteristics in humans. Therefore, one requires a dissolution method mimicking in vivo or the GI tract environment (particularly that of the intestinal). Commonly, this in vivo environment for dissolution testing purposes is represented by three variants: (i) temperature (37 ºC); (ii) an aqueous-based solvent/medium; (iii) a container or vessel with a stirrer to provide interaction between product and solvent.
Another requirement, which is perhaps the most critical one and is often overlooked, is that the method or testing environment must also be product independent, as does the GI tract environment.
It is further important to note that the method to be used must have already been developed and validated independently of the underdevelopment product. On the other hand, it is common for people to use or develop product-dependent dissolution methods. However, unfortunately, such a practice is neither scientifically valid nor correct. Furthermore, the use of a product-dependent method cannot provide true or actual dissolution characteristics of the product (link).
At present, none of the commonly suggested/recommended testers/methods, including pharmacopeial, provide common and/or product independent methods or experimental conditions. Thus such tests/methods cannot provide scientifically valid and/or true dissolution characteristics of a product during the product development stage.
This present-day limitation can easily be addressed by using the crescent-shaped spindle set at 25 rpm with 900 mL of water maintained at 37 ºC. A small amount of solubilizer may be added to water/medium if the drug is low aqueous solubility. For more details regarding the advantages of using a crescent-shaped spindle, please follow the link.
