The stated and promoted mandate of regulatory authorities, including pharmacopeias, is to ascertain that consumers and patients receive safe, efficacious, quality pharmaceutical products such as tablets and capsules. It is important to note that at the commercial manufacturing stage, the safety and efficacy of the products are not usually monitored, only the quality which acts as a surrogate for the safety and efficacy. Therefore, authorities can only claim that they are establishing or monitoring the quality of the products, and by extension products would be considered safe and efficacious. From the industry perspective (both brand-name and generic), it is, in fact, a relatively simple and standard exercise of manufacturing fine chemicals and their composites. This follows the same or similar scientific/manufacturing principles and practices for manufacturing any other chemical or its products.
Considering the strong hold of the authorities, manufacturers and distributors can only sell or import/export products that would meet the regulatory/pharmacopeial requirements and/or standards, i.e., they have to be in compliance. In this regard, it should be important and critical to note that “quality of the products” or “product quality” is an undefined term or parameter, and thus cannot be determined or established. Therefore, claims made by the authorities and/or pharmacopeias for establishing quality are not correct or truthful.
The main reason for this false claim or practice is that the authorities consider and promote compliance as quality, which is incorrect. At present, compliance is not linked to the quality of the products (as it is undefined) but to numerous self-created arbitrary, flashy, and catchy phrases (considered as requirements/standards/practices). They are data Integrity (DI), risk based-assessments, Real World Evidence (RWE), Quality by Design (QbD), Process Analytical Technologies (PAT), regulatory perspectives, precision medicines, patient-centric, and many others. However, the fact remains that none of these requirements and practices has any link to the quality of the products (logically or scientifically) as “quality” is an undefined parameter – but confusing and frustrating vocabulary and mumbo-jumbo for regulatory purposes.
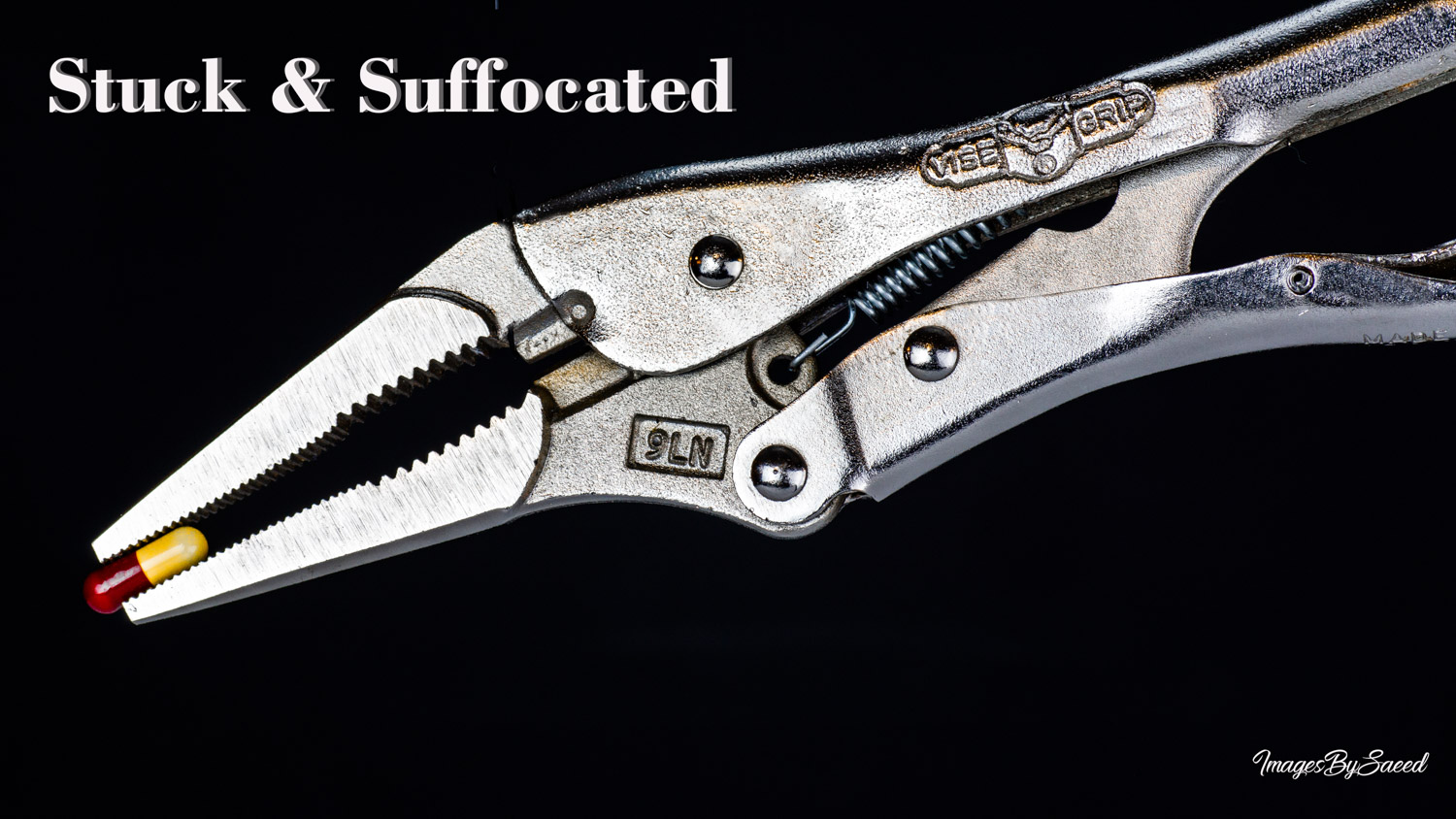
This arbitrariness in setting standards and requirements has choked manufacturing and severely restricted access to actual quality products for patients at affordable prices. One of the main reasons for this manifestation is the implementation of arbitrary standards/requirements through facility inspections by “experts” internal or external to the authorities through so-called GMP practices and/or the implementation of other guidelines. Many of these “experts” may, in reality, be characterized as “snake oil salesmen or women” applying “laws” by choosing or picking some “exploitable,” mostly superficial deficiencies (“observations”), to bad mouth the industry and its staff. On the other hand, the industry and the staff watch and bear this absurdity and humiliation with horror without any options of being heard or reacting. The industry has no choice but to bow down to survive – hence the fraud continues with a vengeance and “gained admiration/credibility” of the “experts.”
In short, it is not possible for public to have quality drug products until authorities start setting logical and science-based standards and specifications. As a start, the “quality” of products needs to be defined clearly with a measurable parameter using valid scientific principles. The irony is that if relevant science and its principles are to be followed, these issues can easily be addressed. This not only would result in reducing the regulatory burden but also provide freedom to the industry for manufacturing quality products as well as open the doors for innovations for affordability and accessibility. I describe such concerns and potential solutions in extensive details through my blog (link) and would be happy to explain these in person as well if it helps. Some suggested blog articles:
(1) Promoting quality standards for drug products: Scientifically speaking, please be systematic and logical! (link)
(2) Possible interpretation of the FDA response to my Citizen Petition – a positive and encouraging development (link).
(3) Pharmaceutical product manufacturing as per current regulatory requirements! (link).
(4) Consumers and patients must wait, and suffer, for the availability of quality pharmaceutical products such as tablet/capsule as well as their genuine and affordable prices. The reason may surprise you! (link).
(5) Comparing Quality Standards – Pharmaceutical vs Consumer Products (link).